Methicillin-resistant Staphylococcus aureus
There is a lot of talk around the world about introducing new categories to describe the degree of infection in chronic wounds e.g. ‘critical colonisation.’
I wonder if we should just get an understanding of the basics i.e. transmission of organisms and cross-infection and correct that first because it is a lack of understanding that kills patients!
A major culprit in cross-infection in all types of healthcare facilities is methicillin-resistant Staphylococcus aureus (MRSA). It is endemic in tertiary referral hospitals in the developed world. [1] The first Australian isolation was made at the Royal Prince Alfred Hospital (RPAH) in Sydney, Australia , in 1965. [2]
So what is MRSA and how can we stop the spread of this potentially deadly nosocomial (hospital acquired) pathogen that has become resistant to so many antibiotics? It is a problem particularly for susceptible patients: neonates, immune suppressed and those undergoing surgical procedures. It can cause infection in wounds, urinary tract, blood and lungs to name but a few sites in the body.
Staphylococcus aureus, which ordinarily lives in the nose and skin of humans, is a harmless berry-shaped (cocci) organism.
Staphylococcus aureus causes problems when it enters what is normally a sterile body site e.g. the bloodstream, urinary tract and wound tissue. If the host (the patient) cannot destroy the numbers of bacteria the result may be, for example, a bloodstream infection (bacteraemia), a urinary tract infection or a wound infection. A wound may exude frank pus as seen in this pressure ulcer.
In fact Staphylococcus aureus was discovered in pus from surgical abscesses in Scotland in 1880 by Sir Alexander Ogston, a surgeon but it was many decades before penicillin became available to treat patients.
PENICILLIN
When penicillin became available in the early 1940s the prognosis for patients with staphylococcal infection improved radically. Unfortunately within a couple of years the first penicillin-resistant staphylococci were recognized, first in hospitals and subsequently in the community. [3] Resistance to penicillin continued to grow, prompting scientists to develop methicillin, the first semi-synthetic penicillinase-resistant penicillin in 1961. Soon after its introduction however, there were reports of methicillin-resistant Staphylococcus aureus (MRSA). [4]
HOW IS MRSA SPREAD?
You are probably all aware that one of the main ways that cross infection occurs is poor hand hygiene. When healthcare workers move from one task or patient (e.g. bed-making) to another (e.g. changing a wound dressing) without hand-washing or hand-rubbing with an alcohol based solution*, pathogenic (disease causing) organisms such as MRSA can be spread andcan be deadly!
(* see hand hygiene, infection control and bed-making )
But when you think about it, unclean hands are only one mode of spread. Anything; bed-linen, clothing, sphygmomanometer cuffs, tourniquets, rolls of tape used to secure dressings — any object that can harbor pathogenic microorganisms (e.g. MRSA) can serve as an agent of transmission of infection.
Collectively these objects are known as ‘fomites’. Look at all the fomites that are used on patient after patient and NEVER CLEANED!!! —- tourniquets and sphygmomanometer cuffs…
Mary Beard demonstrated, in 1969, how new sphygmomanometer cuffs became highly contaminated with pathogenic micro-organisms soon after their introduction into wards at RPAH. [5] Still, they are never washed between patients. I have never known of any healthcare facility where routine practice is for patients to have their own clean sphygmomanometer cuffs (until they acquire MRSA- then they are isolated with their own equipment) …..Strange!!! Seems a bit back-to-front to me!!
‘When such a potential source of sepsis is unrecognized the risks of transmission become magnified as no steps are taken to minimize them.’ [5]
We give patients clean sheets and clean gowns. There would be an outcry if ever we used the same unwashed gown on two patients never mind hundreds or thousands of patients! Yet the same sphygmomanometer cuff is wrapped around arm after arm after arm… gathering more and more bugs.
And 40 years after Beard’s [5] research , testing again carried out at RPAH, showed MRSA to be present not just on sphygmomanometer cuffs and tourniquets, but on scissors, sink basins, taps, soap dispensers and the nurses station. [1] So even the most diligent healthcare worker who washes his or her hands has no hope of stopping cross-infection if they have to handle dirty equipment!
References
1. Barakate MS. Harris JP. West RH. Vickery AM. Sharp CA. Macleod C. Benn RA. A prospective survey of current methicillin-resistant Staphylococcus aureus control measures. Australian and New Zealand Journal of Surgery. 1999; 69(10):712-6, Oct.
2. Barakate MS. Yang YX. Foo SH. Vickery AM. Sharp CA. Fowler LD. Harris JP. West RH. Macleod C. Benn RA. An epidemiological survey of methicillin-resistant Staphylococcus aureus in a tertiary referral hospital. Journal of Hospital Infection. 2000; 44(1):19-26, Jan.
3. Rammelkamp CH, Maxon T. Resistance of Staphylococcus aureus to the action of penicillin. Proc. Royal Soc. Exper. Biol. Med. 1942;51:386–389.
4. Jevons MP. “Celbenin”-resistant staphylococci. Br. Med. J. 1961;1:124–125.
5. Sphygmomanometers as a reservoir of pathogenic bacteria. Beard MA. McIntyre A. Rountree PM. The Medical Journal of Australia 1969; 2: 758
HiCare™ Bath, Making Beds & Infection Control
We have introduced the HiCare ™ Bath technology elsewhere on this site and have said that one advantage of bed-bathing patients using HiCare ™ Bath cloths is that the sheets don’t get wet, as they do with conventional bed-bathing and bowls of water.
When you think about it the [conventional] bowl of water, to bed-bath a patient, rapidly becomes a ‘bacteria soup’ as soon as you dip the washcloth into the bowl.
Bugs are being transferred from one part of the body, to every other part as you move the washcloth from the face to the feet!! Then you have to carry the bowl to the pan-room to pour the [bacteria soup] water out – aerosolising the water and the bugs!!
Who needs it? Use HiCare ™ Bath instead. Sheets may not need to be changed and laundered — saving time, money and water!
Not having to change sheets means there are fewer opportunities for micro-organisms to be dispersed into the air as sheets are pulled off the bed and (thrown!) into the linen skip.
Micro-organisms flying through the air will land on you, the other patients, curtains, trolleys and fomites such as tourniquets and sphygmomanometer cuffs.
Read more about these infection control issues on this website, in particular fomites and methicillin-resistant Staphylococcus aureus (MRSA) , a major culprit in cross-infection.
Meanwhile a few tips to reduce cross-infection when changing sheets:
Why not print off the table & paste it in the linen cupboard, pan room – give each of your staff a copy!! Help them to help themselves.
| Do’s | Don’ts |
| • Remove sheets from the bed slowly – keep the bugs in | • Do not pull sheets off the bed at speed – this will disperse bugs |
| • Place in linen skip slowly | • Do not throw sheets into the skip |
| • After removing sheets from the bed, clean your hands with a waterless ethanol gel /liquid | • Don’t touch the clean sheets until you have cleaned your hands with a waterless ethanol gel /liquid |
| • If the sheets are wet/soiled with urine, blood, faeces etc, wash your hands under running water first | • Do not touch anything with hands that have been in contact with urine, blood, faeces etc.– this will just spread bacteria |
| • Keep clean & dirty linen separate (trolley & skip) | • Do not balance clean sheets on top of the dirty skip to push around |
| • Please put pillows and bedspreads on a chair | • Don’t put pillows and bedspreads on the floor or another patient’s bed |
Why use an alcohol gel handrub?
- The concentration of ethanol will kill bacteria on the hands without making your skin dry and sore
- I find the alcohol gel is much kinder to my skin.
- Using ethanol gel is equal, or superior, to hand washing liquid & water
- It’s fast – rubbing an ethanol gel on your hands between every patient care activity takes a matter of seconds
- Going to a hand-basin to wash and dry hands takes much longer – perhaps that is one reason why it isn’t done as often as it should be
HiCare ™ Bath
This is the first (& only) paid advertisement for a product on The Wound Centre ® website. We have accepted this advertisement on the HiCare ™ Bath system for many reasons:
• It is a wonderful skin-cleansing product
• It is an Australian product
• Australia is suffering from a water-shortage (as many of you in other countries may be also) therefore the timing is perfect to launch this
wonderful product.
• It replaces the traditional bed-bath where nurses carried (OH&S issue) bowls of water which really are a bacteria soup (infection
control issue!)
• HiCare™ Bath washcloths save time
• Towels are not required therefore laundry costs are reduced
• Sheets won’t get wet, as they do during a bed-bath, therefore may not need changing as often, again reducing laundry costs
• It is a wonderful alternative for patients who find showering simply exhausting (those with respiratory disorders)
• For the frail aged at risk of skin tears (manual handling risk – OH&S)
• For those with dementia who may be terrified in the shower and sustain skin tears as a result.
To discuss further just contact Neil at Human Technologies:
Tel: (61) 2 4325-0996 or 1300 653673
Fax: (61) 2 4324-3997
e-Mail: hutek@bigpond.net.au
Web: www.humantechnologies.net.au
National launch of HiCare™ Bath – for ‘no water’ patient bathing
Introduction
HiCare™ Bath is an Australian owned and developed disposable pack of washcloths for bathing patients. The washcloths are impregnated in a pH friendly soap free solution which contains surfactant cleansers, emollients, Vitamin E, an alcohol free fragrance and treated de-ionised water. There is only one chemical preservative (found in some brands of contact lens solutions).
The thick, disposable non-woven, practical size, soft cloths are available in sealed packs of 8 cloths for a full bath or 4 cloths for a birdbath/post op wash. The packs can be micro-waved for a warm bed-bath, cooled, or used at room temperature depending upon patient preference. As well as being very gentle on the skin, the solution also removes pre-operative skin antiseptic solutions.
Indications for use
The HiCare™ Bath washcloths are an alternative to the traditional ‘sponge bath’. They are designed for patients who cannot be showered or when showering is unsafe. For example, patients in high dependency and palliative care units, those suffering cognitive impairment who display resistive behaviours and patients with respiratory disorders who become exhausted in the shower because they simply cannot breathe.
We believe that using HiCare™ Bath can reduce the potential for back injury in staff by providing an alternative to lifting and manoeuvring patients in and out of the shower. We are also convinced that the incidence of skin tears, an increasing problem for the frail-aged, will decrease because manual handling can be reduced.
Cost Savings
HiCare™ Bath is the ideal ‘no water’ solution in those countries with water restrictions. Using HiCare™ Bath washcloths will result in considerable reductions in bathing time and costs. Towels are not required and the need to frequently change bed-sheets is reduced therefore laundry bills will be slashed.
Independent Qualitative and Quantitative Repeat Skin Patch Testing in the USA
The HiCare™ Bath solution was independently tested by Cantor Research Laboratories in the USA in 2005. Testing involved 52 people of different ages and races. No sensitivity or allergic reactions were reported. A full report or one page document is available (e-Mail upon request hutek@bigpond.net.au).
The future
International: Human Technologies (Aust) Pty Ltd intend to seek expressions of interest for the importation of HiCare Bath into other global markets this year.
Domestic: Human Technologies (Aust) Pty Ltd have a distributor network in each State of Australia and sell direct to the ‘at home’ consumer market for palliative care.
Please contact direct :
Human Technologies (Aust) Pty Ltd.
PO Box 1841,
Gosford NSW 2250
Australia
Tel: (61) 2 4325-0996 or 1300 653673
Fax: (61) 2 4324-3997
e-Mail: hutek@bigpond.net.au
Web: www.humantechnologies.net.au
Diabetic Vignettes
‘I marvel that society will pay a surgeon a great deal of money to amputate a limb but nothing to save it’
George Bernard Shaw
I have seen many patients with diabetes mellitus (DM) who have foot ulcers. Some have been so bad as to require amputation of one or both lower limbs. Yet our focus really should be on preservation of the lower limbs, rather than trying to treat the ulcers. Everyone with diabetes should receive basic foot-care education, and regular foot examinations. Foot examinations can be done very simply. Check out this fabulous informative site from an Australian podiatrist :www.2foot.com.au
I want to share a few interesting pieces from papers found on Medline. I urge you all to read the full texts because the information is not only fascinating but scary. Could the increase in the number of patients with DM mean that there will be an increase in the numbers with foot ulcers leading to amputation?!
|
| Amputation of one limb increases the risk of loss of the second limb and is associated with a 50% five-year mortality.
Ref: Apelqvist J, Larsson J, Agardh C-D. Long term prognosis for diabetic patients with foot ulcers. J Intern Med 1993; 233: 485-491. |
| 30% of diabetic patients have contralateral limb amputation within 3 years of the first amputation.
Ref: Most RS, Sinnock KP. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes Care 1983; 6:87–91 |
Peripheral neuropathy, peripheral vascular disease deformities of the feet and infection can lead to ulceration and / or amputation.

Note the ‘clawed toe deformity’ of this diabetic patient.

This patient with peripheral neuropathy presented with a large foreign body in the plantar aspect of the foot and life-threatening infection. The three middle toes required amputation together with deep debridement. The wound healed remarkably!
(Photographs from personal collection)
The risk for the development of ulceration can be assessed by basic clinical examination of the foot. Anyone can learn to do it! Family members, nursing and medical staff, podiatrists, personal care assistants and assistants in nursing in aged care facilities can learn how to do it!! Just use the teaching tools and assessment tools on this excellent website. www.2foot.com.au
Pressure ulcers; what causes them and what prevents them?
Unrelieved pressure over any part of the body for any period of time can cause pressure ulcers. That period of time is different for each patient. It can be a matter of minutes to hours but it is easy to understand.
Anyone who cannot reposition himself or herself; anyone who cannot roll from side to side in bed or get in and out of a bed or chair for example, is at risk of pressure ulcer development.
When somebody cannot move to change position this results in unrelieved pressure in the tissues and blood vessels that are sandwiched between the bony skeleton and a static surface such as a bed or chair. Immobility or decreased mobility is the only evidence-based risk factor for pressure ulcer development.
Patients with diabetes that cannot move themselves and who have no feeling in their feet because of peripheral neuropathy are at risk of heel pressure ulcers in particular, not only because of their immobility but because they may not be able to feel the pain of pressure, therefore may not change position.
The patient that can neither move nor communicate e.g. cannot speak following a stroke, cannot tell you about the pressure pain they feel in their buttocks when sitting for just a few minutes in a chair, is at risk.
Slide 1 Normal Body Reaction to the Effects of Gravity
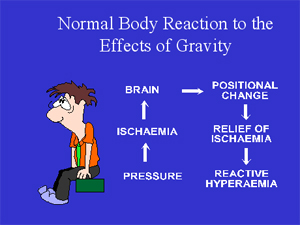
The tissue (skin, fat, muscle, blood vessels etc.) between the ischial tuberosities (the bones in the buttocks) and the seat surface are compressed in a normal healthy person, like Fred and in sick patients, so that there is an extensive area of ischaemic (totally bloodless) tissue. Ischaemic tissue is not good for the body.
Messages go to the brain, which responds by making Fred move (usually subconsciously). THERE IS COMPLETE RELIEF OF PRESSURE, blood surges into the previously ischaemic tissue in the reactive hyperaemic response and any damage resulting from the ischaemia is repaired, in a healthy person.
Now the body rests on a different set of pressure points. A few minutes later this all happens again; Fred moves and there is reperfusion of the area of tissue previously under pressure. The alternate application and then removal of pressure to the tissue covering our bony prominences is as normal as expiration follows inspiration. But what happens to the sick patient who cannot move?
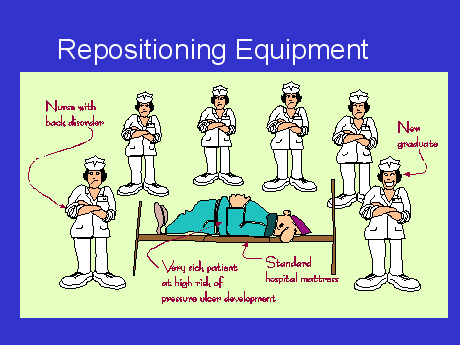
SLIDE 2 Repositioning Equipment.
SLIDE 3 The Viaclin ™ Alternating pressure air mattress (APAM)

There are a couple of wonderful mattresses that I recommend: the Nodec A™ and the Viaclin ™ for the majority of patients in hospital, the community and in nursing homes. A major advantage of the Viaclin ™ alternating pressure air mattress overlay is that it ties on top of the existing mattress.
There is no need for nurses to lift the existing mattress off the bed (an OH&S issue), to drag it down to a storage area (which many facilities do not have) in order to put a full APAM replacement on the bed.
If the patient is on an APAM there is no need for nurses to wake them up to carry out the traditional ‘2-hourly PAC’ regime to prevent pressure ulcers.You have to try to imagine it yourself – being woken from a deep sleep every night for months and years on end (remember having to wake up to breastfeed your babies – all the mothers reading this!!!!).
If the patient is asleep when you do your rounds they should be left to sleep. On the other hand if they are lying awake they can be repositioned. This helps with lung perfusion, joint mobility and provides a change of scene. If you work in the community or a nursing home your patients may be with you for months and years therefore they should not be woken from sleep to be repositioned. Sleep deprivation is harmful to normal metabolism. Nurse them on an APAM. Fewer episodes of repositioning patients also means fewer back injuries for nurses!!
Having an APAM is wonderful for patients cared for by family in their homes. NOBODY need lose sleep! I have met many elderly people who have been told, by health professionals, to reposition an equally elderly spouse every two hours in order to prevent pressure ulcers!! HOW HARD IS THAT? Neither gets any sleep. And when the patient does get a pressure ulcer the elderly spouse is blamed for it!!! The guilt suffered is impossible to imagine. If health professionals can’t prevent pressure ulcers how can we expect an elderly spouse to prevent them?
There are, of course exceptions to this idea of leaving patients to sleep. If the patient has a chest infection the physiotherapist may want the patient to be repositioned frequently during the period of illness.
There are contraindications for the use of APAM’s. Patients with unstable spinal fractures for example cannot be nursed on a moving surface. Decisions for care should always be multidisciplinary.
SLIDE 4 Checklist for high efficiency alternating pressure air mattresses.
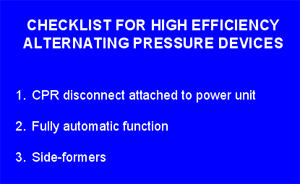
With limited budgets, healthcare facilities need therapeutic equipment that performs as expected. The high output alternating air devices increase tissue perfusion beneath the bony prominences and prevent pressure ulcers and may heal established pressure ulcers. (I have certainly seen elderly, dying patients whose pressure ulcers have healed whilst on the Viaclin ™). I have NEVER known a patient to develop a pressure ulcer whilst nursed on a Viaclin ™.
SLIDE 5 Sideformers on the Viaclin ™.
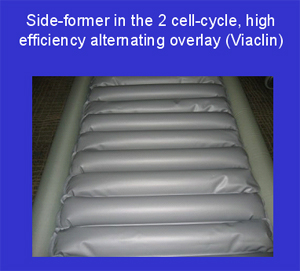
Only high output compressors with air to spare can provide the luxury of side-formers. Side formers prevent the edge of the mattress from collapsing when nurses are trying to get the patient out of bed. Nurses have been known to really hurt their backs trying to hold up patients who slip unexpectedly off the edge of the bed. Sideformers can also prevent the patient getting stuck between the bed rails and the mattress.
SLIDE 6 Cardio-pulmonary resuscitation (CPR) pull.
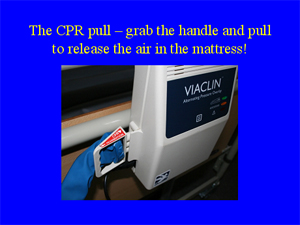
In the event of a cardiac arrest it is important to not only be able to FIND the CPR pull (many are hidden under the mattress) but that once it is pulled the mattress deflates as quickly as possible. The Viaclin ™ CPR pull is easy to see and deflates quickly.

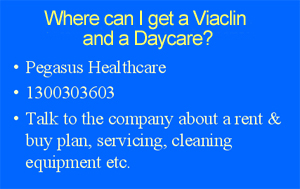
The added extra that I recommed is the Daycare Alternating Pressure Air Cushion. If the patient is at risk of Pressure Ulcers and they need an Alternating Pressure Air Mattress, then it makes sense to provide them with an equivalent when sitting out of bed.
One motor serves both the Alternating Pressure Air Mattress and the Alternating Pressure Air Cushion.
(I have not been paid by Pegasus to promote their products.)