Diabetic Vignettes
‘I marvel that society will pay a surgeon a great deal of money to amputate a limb but nothing to save it’
George Bernard Shaw
I have seen many patients with diabetes mellitus (DM) who have foot ulcers. Some have been so bad as to require amputation of one or both lower limbs. Yet our focus really should be on preservation of the lower limbs, rather than trying to treat the ulcers. Everyone with diabetes should receive basic foot-care education, and regular foot examinations. Foot examinations can be done very simply. Check out this fabulous informative site from an Australian podiatrist :www.2foot.com.au
I want to share a few interesting pieces from papers found on Medline. I urge you all to read the full texts because the information is not only fascinating but scary. Could the increase in the number of patients with DM mean that there will be an increase in the numbers with foot ulcers leading to amputation?!
|
| Amputation of one limb increases the risk of loss of the second limb and is associated with a 50% five-year mortality.
Ref: Apelqvist J, Larsson J, Agardh C-D. Long term prognosis for diabetic patients with foot ulcers. J Intern Med 1993; 233: 485-491. |
| 30% of diabetic patients have contralateral limb amputation within 3 years of the first amputation.
Ref: Most RS, Sinnock KP. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes Care 1983; 6:87–91 |
Peripheral neuropathy, peripheral vascular disease deformities of the feet and infection can lead to ulceration and / or amputation.

Note the ‘clawed toe deformity’ of this diabetic patient.

This patient with peripheral neuropathy presented with a large foreign body in the plantar aspect of the foot and life-threatening infection. The three middle toes required amputation together with deep debridement. The wound healed remarkably!
(Photographs from personal collection)
The risk for the development of ulceration can be assessed by basic clinical examination of the foot. Anyone can learn to do it! Family members, nursing and medical staff, podiatrists, personal care assistants and assistants in nursing in aged care facilities can learn how to do it!! Just use the teaching tools and assessment tools on this excellent website. www.2foot.com.au
Pressure ulcers; what causes them and what prevents them?
Unrelieved pressure over any part of the body for any period of time can cause pressure ulcers. That period of time is different for each patient. It can be a matter of minutes to hours but it is easy to understand.
Anyone who cannot reposition himself or herself; anyone who cannot roll from side to side in bed or get in and out of a bed or chair for example, is at risk of pressure ulcer development.
When somebody cannot move to change position this results in unrelieved pressure in the tissues and blood vessels that are sandwiched between the bony skeleton and a static surface such as a bed or chair. Immobility or decreased mobility is the only evidence-based risk factor for pressure ulcer development.
Patients with diabetes that cannot move themselves and who have no feeling in their feet because of peripheral neuropathy are at risk of heel pressure ulcers in particular, not only because of their immobility but because they may not be able to feel the pain of pressure, therefore may not change position.
The patient that can neither move nor communicate e.g. cannot speak following a stroke, cannot tell you about the pressure pain they feel in their buttocks when sitting for just a few minutes in a chair, is at risk.
Slide 1 Normal Body Reaction to the Effects of Gravity
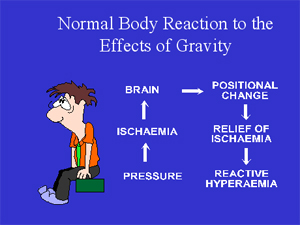
The tissue (skin, fat, muscle, blood vessels etc.) between the ischial tuberosities (the bones in the buttocks) and the seat surface are compressed in a normal healthy person, like Fred and in sick patients, so that there is an extensive area of ischaemic (totally bloodless) tissue. Ischaemic tissue is not good for the body.
Messages go to the brain, which responds by making Fred move (usually subconsciously). THERE IS COMPLETE RELIEF OF PRESSURE, blood surges into the previously ischaemic tissue in the reactive hyperaemic response and any damage resulting from the ischaemia is repaired, in a healthy person.
Now the body rests on a different set of pressure points. A few minutes later this all happens again; Fred moves and there is reperfusion of the area of tissue previously under pressure. The alternate application and then removal of pressure to the tissue covering our bony prominences is as normal as expiration follows inspiration. But what happens to the sick patient who cannot move?
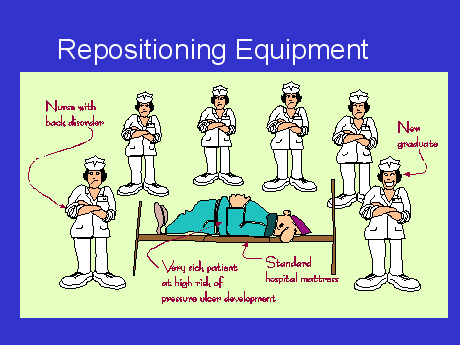
SLIDE 2 Repositioning Equipment.
SLIDE 3 The Viaclin ™ Alternating pressure air mattress (APAM)

There are a couple of wonderful mattresses that I recommend: the Nodec A™ and the Viaclin ™ for the majority of patients in hospital, the community and in nursing homes. A major advantage of the Viaclin ™ alternating pressure air mattress overlay is that it ties on top of the existing mattress.
There is no need for nurses to lift the existing mattress off the bed (an OH&S issue), to drag it down to a storage area (which many facilities do not have) in order to put a full APAM replacement on the bed.
If the patient is on an APAM there is no need for nurses to wake them up to carry out the traditional ‘2-hourly PAC’ regime to prevent pressure ulcers.You have to try to imagine it yourself – being woken from a deep sleep every night for months and years on end (remember having to wake up to breastfeed your babies – all the mothers reading this!!!!).
If the patient is asleep when you do your rounds they should be left to sleep. On the other hand if they are lying awake they can be repositioned. This helps with lung perfusion, joint mobility and provides a change of scene. If you work in the community or a nursing home your patients may be with you for months and years therefore they should not be woken from sleep to be repositioned. Sleep deprivation is harmful to normal metabolism. Nurse them on an APAM. Fewer episodes of repositioning patients also means fewer back injuries for nurses!!
Having an APAM is wonderful for patients cared for by family in their homes. NOBODY need lose sleep! I have met many elderly people who have been told, by health professionals, to reposition an equally elderly spouse every two hours in order to prevent pressure ulcers!! HOW HARD IS THAT? Neither gets any sleep. And when the patient does get a pressure ulcer the elderly spouse is blamed for it!!! The guilt suffered is impossible to imagine. If health professionals can’t prevent pressure ulcers how can we expect an elderly spouse to prevent them?
There are, of course exceptions to this idea of leaving patients to sleep. If the patient has a chest infection the physiotherapist may want the patient to be repositioned frequently during the period of illness.
There are contraindications for the use of APAM’s. Patients with unstable spinal fractures for example cannot be nursed on a moving surface. Decisions for care should always be multidisciplinary.
SLIDE 4 Checklist for high efficiency alternating pressure air mattresses.
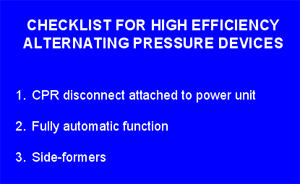
With limited budgets, healthcare facilities need therapeutic equipment that performs as expected. The high output alternating air devices increase tissue perfusion beneath the bony prominences and prevent pressure ulcers and may heal established pressure ulcers. (I have certainly seen elderly, dying patients whose pressure ulcers have healed whilst on the Viaclin ™). I have NEVER known a patient to develop a pressure ulcer whilst nursed on a Viaclin ™.
SLIDE 5 Sideformers on the Viaclin ™.
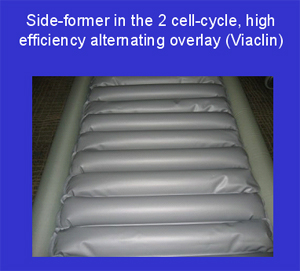
Only high output compressors with air to spare can provide the luxury of side-formers. Side formers prevent the edge of the mattress from collapsing when nurses are trying to get the patient out of bed. Nurses have been known to really hurt their backs trying to hold up patients who slip unexpectedly off the edge of the bed. Sideformers can also prevent the patient getting stuck between the bed rails and the mattress.
SLIDE 6 Cardio-pulmonary resuscitation (CPR) pull.
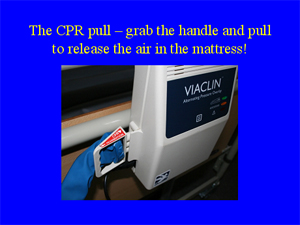
In the event of a cardiac arrest it is important to not only be able to FIND the CPR pull (many are hidden under the mattress) but that once it is pulled the mattress deflates as quickly as possible. The Viaclin ™ CPR pull is easy to see and deflates quickly.

The added extra that I recommed is the Daycare Alternating Pressure Air Cushion. If the patient is at risk of Pressure Ulcers and they need an Alternating Pressure Air Mattress, then it makes sense to provide them with an equivalent when sitting out of bed.
One motor serves both the Alternating Pressure Air Mattress and the Alternating Pressure Air Cushion.
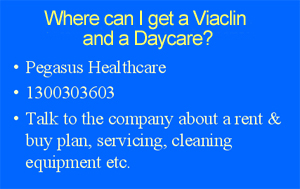
(I have not been paid by Pegasus to promote their products.)
Wound Dressings for the Frail Aged
I personally use, and recommend, ONLY silicone dressings i.e.Mepilex Border™ by Mölnlycke, and Allevyn Gentle Border™ by Smith & Nephew. Both dressings have a wonderful silicone adherent that holds the dressing in place very well but will not damage skin on removal.
The silicone dressings can be left on for a week (depending on the exudates) and I have used it on skin tears, lower limb ulcers and pressure ulcers in nursing home residents.
But how many times have I heard nurses, managers and even wound care colleagues say those dreaded words…Oh! That’s too expensive…when I tell them about the wonderful properties of these, and other, second and third generation wound dressings?
So to help you understand the actual cost of [doing] dressings, I have prepared a spreadsheet. Click here to see it. (you will need Excel on your computer to open it).
The left hand column shows the cost of a traditional daily wound-dressing regime using a dressing pack, impregnated gauze and a secondary dressing held in place with tape.
The right hand column shows the cost of a weekly dressing like Mepilex Border ™ applied immediately after a shower.
Click here for a Step by Step ‘How to Incorporate Your Wound Management into the Residents Shower Regime” (This chart can be printed out and used in your health care facility).
The objective of showering is to clean the wound and surrounding skin. Showering offers a cheap and easy option of copious amounts of water to clean the wound, far more than you would use with a dressing pack and a little pack of normal saline.
Often dressings that are ‘low adherent’ do STICK like glue to wounds! They are painful to remove, can tear the epidermis away from the dermis and create a much larger wound.
Tape used to secure dressings is often contaminated with microorganisms, including methicillin resistant Staphylococcus aureus (MRSA). Tape goes from patient to patient and lives in the fluffy pockets of nurses, around their necks with a bunch of keys and / or it gets thrown back into the cupboard to contaminate all the clean rolls of tape! Scissors used to cut tape may be contaminated with bacteria as well.
These are big infection control issues that are simple to address by just using an ‘all-in-one’ dressing….no tape, no scissors!
In particular for the elderly with their frail tissue paper skin, please think about silicone dressings, it will save their skin at the same time saving you money.
Tinea Pedis & Lower Limb Cellulitis
Did you know that tinea can be spread to many parts of the body eg. the groin, under an abdominal apron and in fingernails. All of this has me questioning the way I was taught to wash and dry patients, whether in bed or in the shower…top to bottom – face before genitals and feet. That makes sense? But what if we are spreading tinea from under the abdominal apron down to the genitals and feet!!
When somebody has tinea pedis (feet) the skin integrity is disturbed allowing bacteria such as Streptococci and Staphylococci to enter, and it is these bacteria that can cause cellulitis. If the tinea is not treated patients may present again and again with lower limb cellulitis. So it is a good idea to check for tinea pedis and treat it, if indeed it is present.
As we don’t always know who has tinea, the elderly, diabetics, and even healthy young athletes, it is time to rethink the whole process.
HiCare bath cloths, warmed in a microwave and disposed of after use…a fresh one for each part of the body. No towels, no wet sheets when bed bathing…that could save on laundry bills.
From an OH&S point of view, HiCare bath cloths would put a stop to the need for bowls of water to be carried to and from the bedside, thus reducing the risk of back injuries. Besides a bowl of water could literally be a bacteria soup – a real infection control issue!
Just by changing the simple practice of bedbathing / showering patients we could see a reduction in tinea and a concomitant reduction in the number of patients presenting with cellulitis of the lower limbs!
A tip to keep sacral hydrocolloids in place.
For years nurses have complained about the sacral hydrocolloids ‘rolling up’ and having to be changed. They may be rolling up because the edge of the dressing has stuck to the draw sheet or the patients’ gown or pyjamas. They stick to some fabrics because the edge of the hydrocolloid dressing is tacky and does tend to pull, or crinkle and roll up. I think most manufacturers’ have, of course, attempted to rectify this by making borders that are much thinner than the centre part of the dressing. Therefore the tacky surface is thinner too.
But once the dressing has rolled up you really must change it. This can be an expensive and unnecessary exercise especially when hydrocolloid dressings are designed to stay on for several days.
A tip to save you $$$’s!
I’m sure you all know that the warmth of your hands will help a hydrocolloid dressing adhere to the patients skin. Once the dressing is applied you need to press all over the hydrocolloid, gently with the palms of your hands, for several minutes.
Now that the hydrocolloid is firmly adherent to the patients skin, you can stop it sticking to the sheets or pyjamas by smearing some moisturiser or talcum powder (just a fingertip full) all around the edge of the dressing. This will take away that sticky edge completely.
This is just one of many little wound care tips I have learnt over the years. A great inspiration and source of knowledge for me, has come from members of the Wound Care Association of New South Wales (WCANSW) Inc. For those of you who live in Australia it is easy to phone committee members if you need advice or want to join the Association. For those of you who live overseas you can email any of the committee or when you visit Australia one day you could tie your holiday in with a conference!! Log on to the WCANSW Inc. website and find out more!